Can Mold Cause A Sinus Infection?
Hello again!
Today, I’m going to go over another topic that comes up frequently in consultations with medical practitioners: mold sinus infections. When I’m looking at results and performing a consult for mold allergy with a practitioner, I frequently see results go up in the first three to six months of treatment. This is very common and likely caused by the mycotoxins’ lipophilic (fat-soluble) chemical properties (1). It could also be because mycotoxins are highly susceptible to reabsorption in the gut via bile acid receptors(2). However, persistent spikes in mycotoxin numbers can still occur after the first six months.
I’ve found that there are two common reasons that this happens: re-exposure from the home or workspace, and infections/colonization of mold in the body. With regards to the latter, one possible location is the gut (see my blog on how mold and mycotoxins affect the gut), and the other main sites are the sinuses and respiratory tract. Although mold has been known to infect the body, surprisingly little research has been done on how mycotoxins are involved. I’d like to take a moment to focus on how mold can cause sinus infections and what has been shown to treat them.
(Let me remind everyone that I’m not an MD, so please seek medical advice before you try and treat yourself!)
Fungal infections of the sinuses are also referred to as Fungal Rhinosinusitis. This classification actually accounts for a spectrum of diseases that are typically caused by organisms including—but not limited to—penicilliosis (now known as taloromycosis), aspergillosis, and fusariosis. These infections are further broken down into either “invasive” or “non-invasive” varieties, depending on weather the fungal hyphae invades tissues through the epithelium (3). The non-invasive types of infections frequently cause chronic rhinosinusitis (also known as chronic sinusitis), which is the presence of pain, facial pressure, and nasal drainage for a period of 12 weeks or more (4). Chronic rhinosinusitis (CRS) is more frequently caused by bacterial sources, which is why practitioners often use antibiotics as a first solution. However, in the cases of fungal infections, antibiotics are not helpful, and I have consulted on many cases where they actually worsened the patient’s symptoms.
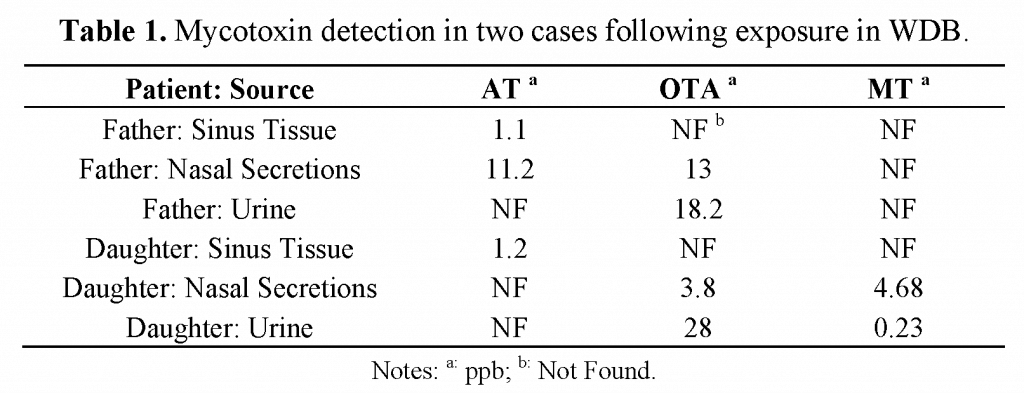
Besides mold infections, the other aspect that can lead to multiple other issues throughout the body is the presence of mycotoxins. Fungal infections (fungal sinusitis) releasing mycotoxins into the body is an area of research which has been vastly ignored by the scientific community. One of the few papers on the subject was published by Brewer et al. (5) (Disclosure: Dr. Dennis Hooper of RTL was an author on this paper). In this paper, they looked at two case studies; in one instance, a father and a daughter both had mycotoxins in nasal secretions AND in their urine. The study also reported on a group of eight CRS patient where seven (87%) had above average mycotoxins, and another group of CRS patients where four out of the eighteen subjects (22%) were positive. Thus, it’s fairly safe to conclude that mold infections are more than capable of releasing mycotoxins into the body.
So, how should these infections be treated? There seems to be several possibilities. Two of the most common options are surgery and antifungals. For some fungal colonies, such as non-invasive fungal balls, surgery seems to be the most common procedure; the fungal material should be macroscopically cleared and the sinus washed out (6).
For other types of fungal infections—both invasive and non-invasive—antifungals should be considered. For non-invasive infections, an intranasal antifungal agent solution, such as amphotericin B, nystatin, or itraconazole could be useful, and previous studies have shown significant improvement in CRS patients using these methods (7). In addition to antifungal nasal sprays, oral antifungals may be necessary. As presented in Brewer et al, one study of 25 patients that possessed mycotoxins in their urine were treated with amphotericin B.
Twenty-two of the patients had a dramatic decrease in their symptoms, which included tremors, ataxia, and vertigo (8).In conclusion, even though a majority of chronic sinusitis is caused by the mold spores bacteria, mold exposure can lead to chronic sinusitis, as well. Methods to determine if your condition is caused by mold would be a urine mycotoxin test or a nasal-swab Fungal DNA test. If you have any questions on this topic, please let us know—our staff is extremely happy to help!
-
- L. Escriva, G. Font, L. Manyes, H. Berrada, Studies on the Presence of Mycotoxins in Biological Samples: An Overview. Toxins (Basel) 9, (2017).
-
- A. Kerkadi et al., Cholestyramine protection against ochratoxin A toxicity: role of ochratoxin A sorption by the resin and bile acid enterohepatic circulation. J Food Prot 62, 1461-1465 (1999).
-
- K. T. Montone, Pathology of Fungal Rhinosinusitis: A Review. Head Neck Pathol 10, 40-46 (2016).
-
- X. Dufour et al., Paranasal sinus fungus ball: epidemiology, clinical features and diagnosis. A retrospective analysis of 173 cases from a single medical center in France, 1989-2002. Med Mycol 44, 61-67 (2006).
-
- J. H. Brewer, J. D. Thrasher, D. Hooper, Chronic illness associated with mold and mycotoxins: is naso-sinus fungal biofilm the culprit? Toxins (Basel) 6, 66-80 (2013).
-
- J. Watkinson, R. Clarke, in Scott-Brown’s Otohinolaryngology and Head and Neck Surgery: Volume 1. (CRC Press, Boca Raton, FL USA, 2018).
-
- J. U. Ponikau et al., The diagnosis and incidence of allergic fungal sinusitis. Mayo Clin Proc 74, 877-884 (1999).
-
- R. JF, G. IH, in Proceedings ofthe 52nd Annual Interscience Conference on Antimicrobial Agents and Chemotherapy Conference. (SanFrancisco, CA, USA, 2013).